Check out my previous posts on IRA price negotiation for drug selection (Part 1) and manufacturer data submission (Part 2).
Today, we will delve into the negotiation process and how CMS will establish the Maximum Fair Price (MFP).
CMS will determine the single price based on the cost of the selected drug per 30-day equivalent supply, weighted across dosage forms and strengths.
The maximum MFP amount will be calculated based on various factors, including plan-specific enrollment weighted amounts and inflation adjustments.
The MFP will be calculated for each NDC-11 for the selected drug, with certain exclusions such as sample packages and NDCs with $0 in covered prescription drug costs.
Claims may be excluded from the MFP refund under certain circumstances, such as prospectively purchased drugs at or below the MFP.
CMS will justify the MFP to manufacturers through a 4-step process, which includes evaluating therapeutic alternatives and unique benefits of the selected drug.
The initial price offer will be based on the net price of therapeutic alternatives, with adjustments made based on various factors impacting clinical benefit, patient outcomes, and usage patterns.
Caregiver experience and cost considerations will also play a role in determining if a treatment is a therapeutic advance.
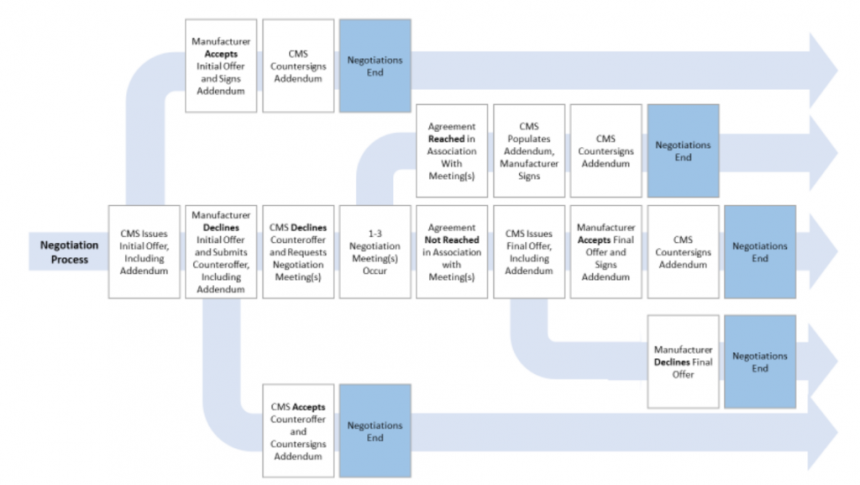
The negotiation process will follow a set procedure outlined in the CMS guidance document. More details can be found in the provided link.
Part 3 – Healthcare Economist